Lower back pain is quite common. It can be caused by both ordinary fatigue and serious injuries and pathologies. If the pain is severe or does not go away after rest, it is important to consult a doctor to rule out dangerous conditions.
What can pain in the lower back be like?
Pain in the lower back can be sharp or aching, appear suddenly or increase gradually, appear with loads or certain movements (for example, bending) or persist regardless of what the person is doing.
The pain can be point-like or radiating (that is, spreading to other areas). In this case, a person has pain not only in the back in the lumbar region, but also in other parts of the body, such as the lower abdomen, perineum, leg or buttock.
Lower back pain may include stiffness of movement or muscle spasms. The person may have difficulty bending or rising from a lying position, standing with a straight back, or maintaining posture when walking.
If the pain is caused by a muscle spasm or a pinched nerve, it can be unbearable and even disabling. Such pain forces you to stay in bed until you receive medical help.
Why does my lower back hurt?
The most common cause of pain in the lower back is one or another pathology of the musculoskeletal system: sprains, pinching, inflammation. They are often found in men who work with their hands, athletes, and young mothers.
Also, discomfort in the lower back can be a sign of acute or chronic diseases of the internal organs. This occurs due to the fact that pain impulses are able to be transmitted along nerve fibers to neighboring regions. In this case, they say that the pain "radiates" to the lower back.
Diseases of the musculoskeletal system causing pain in the lower back
Most often, lower back pain is caused by injuries and pathologies of the musculoskeletal system - muscle and ligament sprains, spinal injuries, herniation and protrusion of intervertebral discs, inflammation of the joints, bone diseases.
Deformations and sprains of muscles and ligaments
Such injuries can occur due to awkward movement if a person lifts something very heavy or does not follow safety precautions when handling bulky objects. You can also get injured while playing sports or if you simply sneeze unsuccessfully.

Lower back pain may occur if you lift heavy objects without following safety precautions.
With sprains and strains, the pain intensifies during movement, and spasms may appear in the muscles. It may be painful for the person to walk, bend forward, or hold their back straight.
Diagnosis of deformation and sprain of muscles and ligaments is based on data from a physical examination and instrumental studies - ultrasound, x-ray, MRI of the lumbar region. If you suspect a sprain or deformation of muscles or ligaments, you should contact an orthopedic traumatologist.
Treatment consists of relieving acute pain and muscle spasms using ice compresses, painkillers, and medications to relieve muscle spasms (muscle relaxants). It is important to give the damaged area rest to allow the tissue to recover - this usually takes about 2 weeks. After this, it is important to begin rehabilitation: physical therapy exercises aimed at restoring muscle function are indicated.
Without treatment, strains and sprains lead to limited mobility: trying not to injure the damaged area, a person reduces activity, which can lead to weight gain, decreased bone strength and loss of muscle mass.
Spinal injuries
Damage (usually a fracture) to one or more vertebrae occurs as a result of falls, accidents, sports, or household injuries. In people with bone density disorders (such as osteoporosis), such damage can be caused by even minor exposures.
Treatment of spinal injuries is to prevent displacement and further deformation of the spinal discs. If the damage is not severe, it is recommended to sleep on a hard surface and limit physical activity. If the damage is significant, surgical methods are used for fixation.
Without treatment, damage to the spinal discs can cause stenosis (narrowing) of the spinal canal, neurological disorders, including sciatica - pinched nerve fibers extending from the spine.
Intervertebral disc pathologies
Intervertebral discs are fibrocartilaginous plates with jelly-like contents located between the vertebrae. They act as shock-absorbing cushions for the vertebrae, ensuring their mobility. Discs can become dislodged (protruded) or ruptured (herniated), causing severe pain and limiting spinal mobility.
Intervertebral hernias and protrusions can occur in people with weak muscles and excess weight, in those who lead a sedentary lifestyle or lift heavy objects. People who smoke are more susceptible to intervertebral disc pathologies.

Intervertebral hernia - protrusion of an intervertebral disc into the spinal canal
Treatment consists of relieving pain and inflammation - rest, painkillers, ointments and compresses on the inflamed area are recommended. The doctor may prescribe physical therapy or exercise therapy. For moderate damage, the disc can recover if the cause of the herniation or protrusion is excluded - for example, strengthening the muscle corset, reducing weight and not putting excessive stress on the spine.
If the pain in the lower back is so severe that it interferes with everyday activities, does not subside within 1–1. 5 months, or if the symptoms worsen, you should contact your doctor again. In some cases, steroid therapy or even surgery may be required. With age, it is possible to develop degenerative disease of the intervertebral discs - they become flatter and perform a worse shock-absorbing function, which can also cause pain. In this case, treatment includes pain relief and general improvement of the body.
Scoliosis of the lumbar spine
Scoliosis (curvature) of the spine is a displacement of the spinal column to the right or left relative to the vertical axis. The pathology leads to increased pressure on certain areas of the intervertebral discs and vertebrae, as well as to pinched tissue and nerve fibers. Scoliosis can cause severe pain in the lower back on the right or left—where most of the stress is placed—and severely limit the mobility of the spine.

Scoliosis (curvature) of the spine can cause severe pain in the area of the lower back where a lot of stress is placed
Scoliosis can occur due to weakening of the muscular corset in the absence of sufficient physical activity, a sedentary lifestyle (in schoolchildren, office workers). In this case, it is difficult for the muscles to maintain the physiological position of the back and curvatures form.
Treatment involves the introduction of balanced physical activity (physical therapy, swimming), massage and manual therapy, physiotherapeutic procedures to strengthen muscles, such as electrical stimulation. For severe injuries, wearing a corset is recommended, which helps maintain the correct position of the spine.
Arthritis and arthrosis
Inflammation and degenerative processes in the joints of the spine can also cause severe lower back pain. There are many forms of arthritis, including osteoarthritis (damage to cartilage and adjacent tissues), ankylosing spondylitis (ankylosing spondylitis - damage to the joints of the spine, which leads to fusion of the vertebrae).
Arthritis can be caused by natural aging, genetic predisposition, or autoimmune diseases.
Treatment of arthritis, depending on its form, may include the use of non-steroidal and steroidal anti-inflammatory and painkillers, physiotherapeutic procedures (magnetic therapy, electrophoresis), therapeutic massage, and physical therapy.

Physiotherapeutic procedures help relieve pain due to joint pathologies
Spondylolisthesis
Displacement of a vertebra relative to the spinal column (spondylolisthesis) occurs as a result of injury or degenerative processes in the spine. The pathology occurs in athletes, older people or people with a hereditary predisposition to bone diseases (for example, osteoporosis - a disorder of bone density). Spondylolisthesis can lead to severe pain in the lower back, buttocks, and legs, and cause cramps or weakness in the legs.
Treatment involves relieving pain and inflammation that occurs due to compression of neighboring tissues by the vertebra. Depending on the severity of the pain syndrome, the doctor may prescribe non-hormonal painkillers in tablets or injections of corticosteroid drugs. At the same time, physiotherapeutic procedures and exercise therapy are prescribed to strengthen the muscles and restore the position of the vertebrae. If spondylolisthesis is accompanied by very severe pain, surgical treatment is used.
In traumatic and non-infectious pathologies of the musculoskeletal system, pain in the lower back usually subsides or decreases when the person takes a comfortable position.

If spondylolisthesis is accompanied by severe pain, your doctor may prescribe corticosteroid injections.
Infectious diseases of the spine
Inflammation of the bone tissue (osteomyelitis) and inflammation of the intervertebral disc (discitis) can cause severe lower back pain. These pathologies, as a rule, are of a secondary nature, that is, they arise as a complication of inflammation of other organs (the infection enters the tissues through the bloodstream).
Treatment involves hospitalization, lasts up to 1 month, and then requires rehabilitation, which takes from 6 to 12 months.
Tumor diseases of the spine
Neoplasms can develop under the influence of hereditary or external factors (for example, radiation), but most often they appear as repeated foci (metastases) in cancer of other organs - lungs, mammary glands, prostate, thyroid gland, kidneys.
One of the most characteristic symptoms of tumor pathologies is pain that does not subside when changing position or after rest. Symptoms such as numbness, partial paralysis, uncontrolled urination and a sharp increase in body temperature with chills are also possible. Without treatment, symptoms worsen.
Treatment is prescribed depending on the type of tumor, its location and symptoms and may include chemotherapy, radiotherapy and surgical removal of tumors. Pain relief is carried out with non-hormonal or steroid drugs. To stabilize the spine, your doctor may prescribe wearing a corset.

Orthopedic corset helps stabilize the spine
Diseases of internal organs causing pain in the lower back
Lower back pain can occur with diseases not associated with pathologies of the spine and adjacent tissues. Acute or aching, it can accompany inflammation of internal organs: pyelonephritis, urolithiasis, abdominal aortic aneurysm. In women, pain in the lower back can develop due to gynecological pathologies.
Urolithiasis disease
A disease in which stones form in the kidneys and bladder - hard formations from the sediment of chemical components of urine. Lower back pain is one of the main signs of pathology. Depending on the size and location, kidney stones can cause a dull and aching pain that occurs and subsides periodically, or a very sharp pain that does not go away on its own and requires emergency medical care.
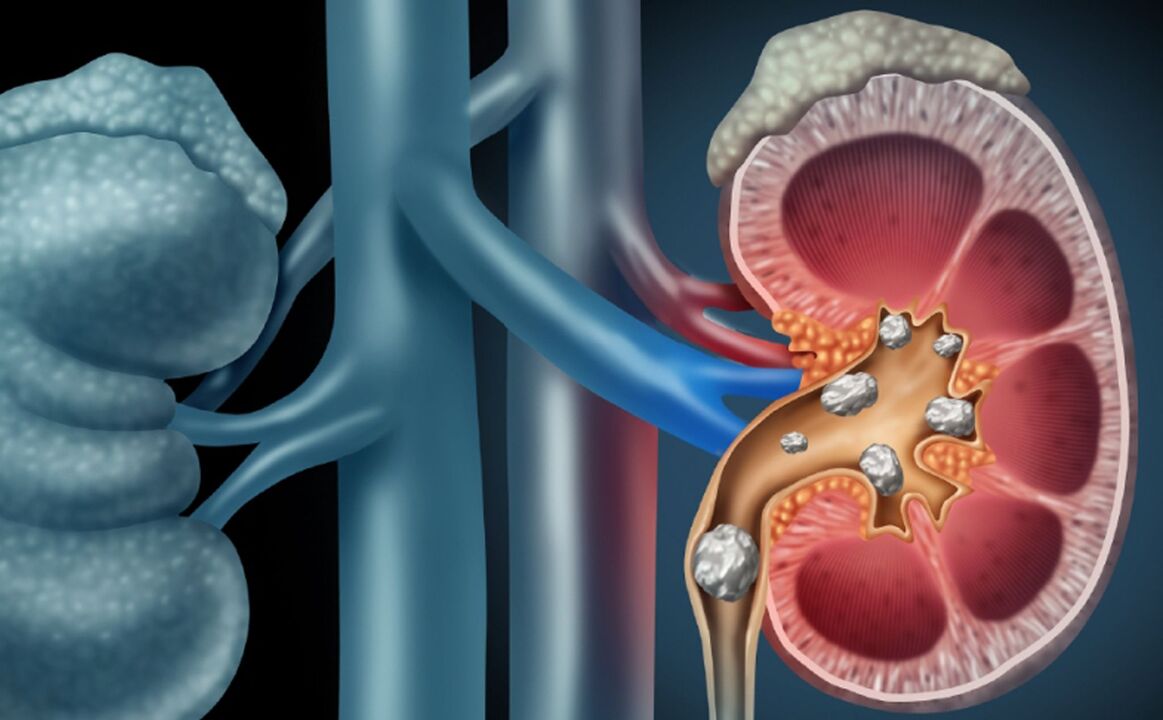
Urolithiasis - the formation of stones in the kidneys and bladder
If you suspect kidney stones, you should contact a urologist or nephrologist. The doctor will prescribe tests and instrumental studies (ultrasound, X-ray examination, computed tomography, including with the use of a contrast agent) to make a diagnosis and choose treatment tactics.
Treatment is prescribed taking into account the size, nature, location of stones and other factors. If the stone is small (5–10 mm) and there are no other indications for surgical removal, drug treatment is used. If there is no positive dynamics within a month, removal by non-invasive or surgical methods is recommended.
Abdominal aortic aneurysm
A weakening of the walls of the abdominal aorta (aneurysm) can lead to life-threatening conditions such as aortic rupture and intra-abdominal bleeding. As a rule, the pathology occurs in older people: the risk group includes men over 65 years of age and women over 70 years of age, including smokers, those suffering from vascular diseases (high blood pressure), having previously had aneurysms or having a hereditary predisposition to them.
Pain in the lower back due to an abdominal aortic aneurysm does not subside over time and may be accompanied by pain in the abdomen and legs.
If an aneurysm is suspected, an abdominal ultrasound and computed tomography are prescribed.
Treatment depends on the size of the aneurysm. Small changes require monitoring with instrumental examination twice a year and lifestyle adjustments. Significant (over 5 cm, with a high risk of rupture) are an indication for abdominal or minimally invasive surgery.
How to prevent lower back pain
Since lower back pain is most often caused by traumatic injury to muscles, fascia, joints or bones, the main recommendation for prevention is to follow safety precautions, maintain a strong muscle corset, as well as healthy bones and joints.
Prevention of sprains and microtraumas of the lower back:
- a varied diet that includes the vitamins and minerals necessary to maintain healthy bone and muscle tissue and joints;
- maintaining a healthy weight;
- regular physical activity: exercises to prevent lower back pain should include strength exercises to develop the muscular frame, stretching to relieve muscle tension and spasms, and cardio training to maintain blood supply and tissue nutrition;
- compliance with safety precautions while playing sports - for example, the first classes in the gym must be supervised by a qualified trainer;
- compliance with safety precautions at home - many injuries can be avoided if you wear comfortable shoes, hold on to the railings on the stairs, take your time when it’s slippery outside;
- observing safety precautions when lifting heavy objects - the load on the spine will be less if you approach the object as close as possible (do not reach for it), and when lifting objects from the floor, bend your legs rather than tilt your body.

Yoga and Pilates classes help relieve spasms and tension in the lower back
Smoking impairs blood circulation and impairs tissue nutrition, increasing the risk of damage and injury.
What to do if your lower back hurts
If your lower back hurts, the reasons may be different, which means the treatment tactics will also be different.
In case of severe physical fatigue, the back needs to be given rest - perhaps this will be enough for the muscles to recover and the mobility of the spine to return.
If the pain does not go away within 1-2 days or if it is very severe, you should consult a doctor. While waiting for a doctor, you can try to relieve acute pain with painkillers.
At the appointment, the doctor will conduct an examination, determine the cause of the pain and give recommendations for treatment. This will help eliminate dangerous conditions and prevent the development of complications.
Warming (lumbar pepper patch, hot water bottle, sauna) is contraindicated for inflammation, but can relieve acute pain in the lower back if it is caused by muscle fatigue or a pinched nerve. These methods can only be used after consulting a doctor.
Which doctor should I contact with a complaint of lower back pain?
If you suspect pathology of the musculoskeletal system, you should contact a neurologist and orthopedic traumatologist.
Diagnosis is carried out during a physical examination and using instrumental methods: magnetic resonance therapy, computed tomography, X-ray and ultrasound. It is also possible to prescribe a myelogram (x-ray or CT study with a contrast agent injected into the spinal canal) and electromyography - a study that allows you to assess the condition of nerve and muscle fibers.
If you suspect kidney disease, you should contact a urologist, nephrologist or therapist. The doctor will analyze the complaints and conduct a physical examination, and then prescribe laboratory and instrumental tests to clarify the diagnosis.
Based on blood and urine tests, the doctor will be able to determine whether there is inflammation in the organs of the urinary system, and ultrasound and x-ray studies will help visualize the organs, determine the cause of pain and choose the most effective treatment tactics.
If the origin of pain in the lower back is unclear, you should consult a general practitioner or therapist.
The doctor will collect an anamnesis (medical history), analyze hereditary risks, conduct a physical examination and prescribe tests that will identify inflammatory processes or disorders in the functioning of internal organs.
A general blood test helps identify the inflammatory process.
If necessary, the doctor will refer you for instrumental studies (ultrasound, x-ray, MRI) or recommend contacting a specialist for further diagnosis and treatment.



















